What does health equity mean? A Close Look at the Battle for Fair Healthcare in the US
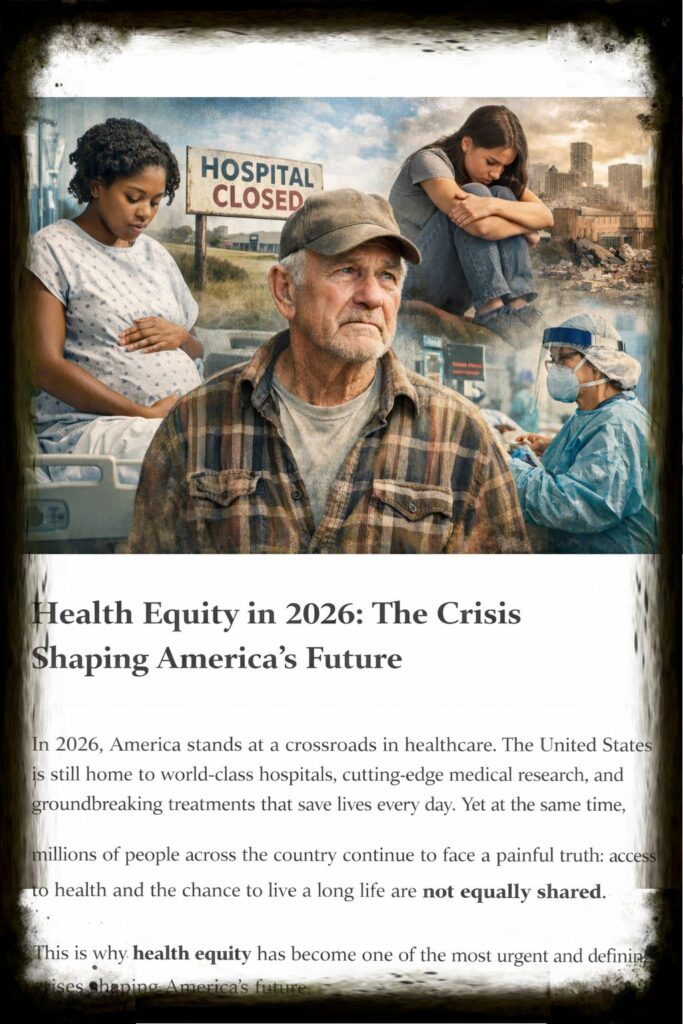
In 2026, America stands at a crossroads in healthcare. The United States is still home to world-class hospitals, cutting-edge medical study, and groundbreaking treatments that save lives every day. However, millions of people across the country still have to face a sad truth: not everyone has the same access to health care and the chance to live a long life. This is why health equity has become one of the most important and pressing problems facing the future of the United States.

Health equity means that every person, regardless of their race, income, neighborhood, gender, or background, has a fair chance to achieve their best possible health. It isn’t just about giving everyone the same tools. It is about understanding that different communities face different barriers, and those barriers must be addressed if America wants a healthcare system that is truly fair.
It’s not a new topic of talk, but in the last few years it’s become louder and harder to avoid. Deep flaws in the system were shown during the pandemic years, and the economic and social forces that followed have only made those holes bigger. There are no longer any figures or academic reports that hide the crisis in 2026. In everyday life, you can see it in places like rural towns that lose hospitals and urban areas where people with chronic illnesses have trouble getting care.
One of the most striking realities about health inequity in America is that where you live can decide how long you live.
Even between neighborhoods that are only a few miles apart, life expectancy can change a lot. People who live in wealthier areas often have access to better schools, safer homes, and preventive care. In poorer areas, families may fight with food insecurity, environmental pollution, unsafe streets, and limited healthcare facilities.
These conditions cause unequal health outcomes long before someone even steps into a doctor’s office.
In 2026, the maternal health disaster remains one of the most heartbreaking examples of health inequity. Black women in the United States continue to face far higher risks of pregnancy-related problems and death compared to white women.
This difference is not explained by biology. It is driven by systemic problems such as unequal treatment, lack of access to quality prenatal care, and the long history of racial bias within medical institutions.
Even highly educated and financially sound Black women are not immune, showing that this problem runs deeper than income alone. The crisis represents a healthcare system that too often fails to protect all mothers equally.
Mental health has also become a defining equity problem for modern America. Anxiety, depression, and stress-related disorders are growing, especially among young people.
Yet access to mental health care remains deeply uneven. In many places of the country, therapy is expensive, mental health professionals are scarce, and insurance coverage is limited.
Communities already dealing with poverty or instability often face the greatest mental health burdens but have the fewest resources available. The result is a hidden epidemic where those who most need care are often least able to receive it.
Rural America marks another front in the health equity crisis. Across the country, rural hospitals have continued to close due to financial pressures and workforce shortages.
For millions of Americans, this means longer travel times for emergency care, fewer experts, and limited access to preventive services. A heart attack, a stroke, or a childbirth emergency becomes far more dangerous when the nearest hospital is hours away. Rural health inequity is not just about inconvenience; it is about life.
Health equity is also shaped by the affordability problem in American healthcare. Even in 2026, medical debt remains a heavy load for countless families. People delay care because they fear the cost. They skip drugs because prescriptions are too expensive. They avoid preventive checkups because they cannot pay insurance deductibles. These financial barriers create a cycle where small health problems become major crises simply because care was out of reach.
Food access is another major driver of inequality. Millions of Americans live in food deserts, places where fresh fruits, vegetables, and healthy groceries are difficult to find.
Instead, fast food and processed meals rule. Over time, this leads to higher rates of obesity, diabetes, and heart disease. In this way, health inequity becomes woven into daily life, shaped not by personal decisions alone but by structural realities.
The climate problem is now also intersecting with health equity in powerful ways. Extreme heat, wildfires, and flooding are hitting vulnerable areas the hardest.
Low-income families are more likely to live in places with poor air quality or limited cooling infrastructure. People with chronic conditions face higher risks during climate disasters, yet often have fewer resources to react or recover. In 2026, environmental health has become inseparable from the fight for equality.
Technology has brought new possibilities, but it has also caused new divides. Telehealth expanded dramatically after the pandemic, giving remote doctor visits and mental health support.
For many, it has improved access. But for others, especially those without reliable internet, smartphones, or digital literacy, telehealth stays out of reach.
The digital divide has become a modern health equity problem, showing that innovation alone cannot solve inequality without inclusive infrastructure.
The root of health inequality lies in what experts call the social determinants of health. These are the situations in which people are born, grow, live, work, and age. Income, schooling, housing, transportation, neighborhood safety, and availability to healthy food all shape health outcomes.
A person cannot simply choose wellness if their surroundings makes wellness nearly impossible. Health equity needs America to address these deeper factors, not just medical care itself.
In response to these challenges, health equality has become a growing priority in public policy and healthcare leadership. Many states have boosted Medicaid coverage, helping millions gain access to insurance.
Community health centers continue to serve underserved areas, offering affordable care where it is needed most. Hospitals are investing in training programs to reduce bias and improve cultural skills. Federal and local efforts are increasingly focused on reducing disparities in maternal care, chronic disease prevention, and mental health support.
Yet the road ahead remains tough. Achieving health equality is not a quick fix. It needs long-term investment, structural change, and national commitment. It means rethinking how resources are distributed, how healthcare organizations treat patients, and how communities are supported beyond the walls of clinics and hospitals.
The health equity problem shaping America’s future is ultimately about more than healthcare. It is about what kind of society the United States wants to be. A country cannot truly thrive when millions are left behind, when life expectancy is determined by race or neighborhood, and when health becomes a privilege rather than a shared right.
In 2026, the fight for health equality is one of the defining moral challenges of the country. It calls for empathy, fairness, and action. It asks America to face uncomfortable truths and build a future where everyone, not just the fortunate, has the chance to live a healthy life.
Health equity is not an abstract idea. It is the difference between prevention and disaster, between survival and loss, between fairness and inequality. And as America goes forward, the question is no longer whether health equity matters. The question is whether the country is willing to do what it takes to achieve it.
Conclusion
As America goes deeper into 2026, the fight for health equity has become more than a policy discussion—it has become a defining test of the nation’s values. In a country with amazing medical innovation, no one should be left vulnerable simply because of their race, income, or ZIP code.
Yet the realities of unequal access, rising prices, rural hospital closures, mental health gaps, and systemic disparities continue to shape the lives of millions.
Health equity is not about giving the same healthcare to everyone—it is about ensuring that every person has a fair chance to live a healthy life, regardless of the barriers they face.
The future of American healthcare rests on whether the nation is willing to tackle these inequalities with urgency, compassion, and long-term commitment.
Because a truly strong healthcare system is not measured by how advanced it is for the privileged, but by how available it is for everyone.
The crisis of health equity is shaping America’s future—and the choices made today will decide whether that future is fair, healthy, and inclusive for all.
Thank you for visiting usaconcern.com and taking the time to read our content. Your visit truly matters to us. Stay alert and stay informed, because an informed voice can help shape a better future.
Feel Free to leave a comment below with your thoughts!!

